Digital Healthcare: Doctor on Call, E-Prescription, and Lab Services

In today’s fast-paced world, access to healthcare services has become more critical than ever. With the advent of technology, several innovative solutions have emerged to make healthcare more convenient and accessible. Among these, “Doctor on Call,” “E-Prescription,” and “Lab Services” are revolutionizing the way patients receive medical care. Let’s explore how these advancements are saving lives and time. Along with understanding what else we can expect soon by the digital healthcare shift. Digital Healthcare – The Transformation Of Technology Digital healthcare refers to the integration of technology into healthcare services, enabling the delivery of medical care and health-related services through digital platforms. This transformative approach to healthcare leverages digital tools, such as mobile apps, wearable devices, telemedicine platforms, and electronic health records (EHRs), to improve access, efficiency, and quality of care for patients and healthcare providers alike. Book Appointment Telemedicine Is Now Just A Call Away! One of the key components of digital healthcare is telemedicine, which allows patients to consult with healthcare professionals remotely via video calls, phone calls, or secure messaging platforms. Telemedicine enables timely access to medical advice, diagnosis, and treatment, particularly for individuals living in rural or underserved areas, those with mobility limitations, or those seeking non-urgent medical care. What Are Electronic Health Records? Electronic health records (EHRs) play a crucial role in digital healthcare by digitizing patient health information and medical records. EHR systems allow healthcare providers to access, update, and share patient data securely, facilitating seamless communication and collaboration among care team members. Patients can also access their health records electronically, empowering them to take an active role in managing their health and making informed decisions about their care. Mobile Healthcare Health apps and wearable devices are increasingly popular in digital healthcare, offering tools for monitoring health metrics, tracking fitness goals, and managing chronic conditions. These digital health tools enable individuals to monitor their health in real-time, receive personalized health insights, and engage in preventive health behaviors. Schedule Your Session with Vesta Care Experts Today! Dial 052 104 6920 Now Remote Patient Monitoring Made Life Easy Another significant aspect of digital healthcare is remote patient monitoring, which involves the use of connected devices to track patients’ health data, such as vital signs, blood glucose levels, or medication adherence, outside of traditional healthcare settings. Remote monitoring allows healthcare providers to monitor patients’ health status remotely, identify potential issues early, and intervene proactively to prevent complications. The New Doc Is AI – Artificial Intelligence Artificial intelligence (AI) and data analytics are also driving innovations in digital healthcare, enabling advanced data processing, predictive modeling, and personalized treatment recommendations. AI-powered algorithms can analyze large volumes of health data to identify patterns, predict disease risk, and tailor treatment plans to individual patients’ needs. Doctor on Call: Bridging the Gap Between Patients and Healthcare Providers Doctor on Call services have transformed the way patients access medical care by providing immediate access to healthcare professionals through phone calls, video consultations, or mobile apps. Whether it’s a minor illness, chronic condition management, or medical advice, patients can consult a doctor from the comfort of their homes, eliminating the need for travel and long wait times at clinics. Benefits of Doctor on Call 1: Immediate Access to Medical Advice In emergencies or after-hours, patients can receive timely medical advice without the need for an in-person visit. 2: Convenience Doctor on Call services offer flexibility in scheduling appointments, making it easier for patients to seek medical assistance around their busy schedules. 3:Cost-Effective By avoiding unnecessary visits to emergency rooms or urgent care centers, patients can save on healthcare expenses while receiving quality care. The Rise of Telemedicine: Transforming Healthcare Delivery Telemedicine, a key component of Doctor on Call services, has gained momentum in recent years, enabling healthcare providers to deliver remote medical care using telecommunications technology. Through secure video conferencing platforms, patients can interact with healthcare professionals, discuss symptoms, receive diagnoses, and even undergo follow-up consultations, all from the comfort of their homes. Worried? Reach Out to Us at info@vestacare.ae for Expert Assistance! Telemedicine in Practice: Enhancing Patient Care Telemedicine has revolutionized various aspects of patient care, including: 1: Chronic Disease Management Patients with chronic conditions such as diabetes, hypertension, or asthma can benefit from regular virtual check-ups and medication adjustments without the need for frequent clinic visits. 2: Mental Health Support Telemedicine offers convenient access to mental health professionals for therapy sessions, counseling, and psychiatric evaluations, reducing barriers to care and stigma associated with seeking mental health treatment. 3: Specialty Consultations Patients living in remote or underserved areas can access specialist care through telemedicine, reducing the need for travel and long wait times for appointments. E-Prescription: Streamlining Medication Management and Patient Safety E-Prescription, also known as electronic prescribing, has transformed the prescription process by allowing healthcare providers to electronically send prescriptions to pharmacies, eliminating the need for paper prescriptions. This technology streamlines medication management, enhances medication safety, and improves medication adherence among patients. Benefits of E-Prescription Indeed, the COVID-19 pandemic accelerated the adoption of technology across various sectors, and healthcare witnessed remarkable transformations. Among the groundbreaking advancements, E-Prescription emerged as a game-changer, revolutionizing the way medications are prescribed, managed, and dispensed. Let’s delve into how E-Prescription is not only meeting deadlines but also saving lives in the process. 1: Accuracy E-prescription reduces the risk of errors associated with handwritten prescriptions, such as illegible handwriting or incorrect dosages, leading to safer medication practices. 2: Efficiency Healthcare providers can quickly transmit prescriptions to pharmacies, reducing waiting times for patients and ensuring timely access to medications. 3: Medication Adherence E-prescription systems maintain a comprehensive record of patients’ medication history, allowing healthcare providers to identify and address medication non-adherence issues promptly. For example, overdose of antibiotics, that we will talk about in the next phase. Your In-Home Doctor, Just a Call Away! Book Your Session Now at 052 104 6920. The Overuse And Misuse Of Antibiotics We see a concerning rise in antibiotic resistance, posing a significant threat to global public health. While antibiotics have undoubtedly
Chronic Pain Management – Your Essential Physiotherapy Guide

Chronic pain is a complex condition that affects millions of individuals worldwide, impacting their quality of life and daily functioning. In this comprehensive guide, we will explore the causes of chronic pain, its management strategies, the role of physiotherapy in treatment, and effective ways to alleviate symptoms. Understanding Unceasing Pain Chronic pain is defined as persistent pain lasting for more than three to six months, beyond the expected time for tissue healing. It can result from various factors, including injury, inflammation, nerve damage, or underlying medical conditions. Common types of chronic pain include back pain, arthritis pain, neuropathic pain, and fibromyalgia. Book Appointment Causes of Never-ending Pain Chronic pain can have numerous causes, including: Injury or Trauma: Previous injuries or trauma to muscles, joints, or nerves can lead to conditions such as low back pain, neck pain, and repetitive strain injuries. Inflammation: Inflammatory conditions such as rheumatoid arthritis, osteoarthritis, and autoimmune disorders can cause constant aching by triggering inflammation and tissue damage. Nerve Damage: Neuropathic pain results from nerve damage or dysfunction, leading to shooting or burning sensations, numbness, and tingling. Conditions such as diabetic neuropathy, sciatica, and post-herpetic neuralgia fall into this category. Underlying Medical Conditions: Unending pain can be a symptom of underlying medical conditions such as fibromyalgia, endometriosis, migraines, and inflammatory bowel disease. Chronic Pain Management And Techniques Managing frequent pain requires a comprehensive approach tailored to individual needs. Treatment strategies may include: Medications: Pain-relieving medications such as nonsteroidal anti-inflammatory drugs (NSAIDs), opioids, antidepressants, and anticonvulsants may be prescribed to alleviate symptoms and improve function. Physical Therapy: Physiotherapy plays a crucial role in prolonged pain management by promoting mobility, strength, and flexibility through exercises, manual therapy, and modalities such as heat and cold therapy, ultrasound, and electrical stimulation. Cognitive-Behavioral Therapy (CBT): CBT helps individuals develop coping skills, change negative thought patterns, and manage stress, anxiety, and depression associated with established distress. Lifestyle Modifications: Adopting a healthy lifestyle, including regular exercise, proper nutrition, adequate sleep, stress management, and smoking cessation, can help reduce pain and improve overall well-being. Interventional Procedures: In some cases, interventional procedures such as nerve blocks, epidural injections, radiofrequency ablation, and spinal cord stimulation may be recommended to target specific pain generators and provide relief. Role of Physiotherapy in Frequent Pain Management Physiotherapy plays a pivotal role in recurring pain management by addressing physical impairments, improving functional capacity, and enhancing quality of life. Key components of physiotherapy treatment include: Assessment and Evaluation: A thorough assessment helps identify the underlying causes of pain, functional limitations, and areas of muscle weakness or imbalance. Individualized Treatment Plan: Based on the assessment findings, a personalized treatment plan is developed, incorporating a combination of exercises, manual therapy techniques, and modalities tailored to the individual’s needs and goals. Exercise Therapy: Exercise programs focusing on stretching, strengthening, and cardiovascular conditioning help improve flexibility, muscle strength, endurance, and overall physical function. Manual Therapy: Hands-on techniques such as joint mobilization, soft tissue massage, and myofascial release are used to alleviate muscle tension, improve joint mobility, and reduce pain. Education and Self-Management: Education on pain management strategies, ergonomic principles, activity modification, and self-care techniques to empower individuals to take an active role in their recovery. Modalities: In addition to exercise and manual therapy, modalities such as heat, cold, electrical stimulation, ultrasound, and traction to relieve pain are used. These reduce inflammation and promote tissue healing. How Does The Chronic Pain Management Help? The goals of physiotherapy include: 1. Pain Relief Doctors use various techniques such as manual therapy, modalities (e.g., heat, cold, electrical stimulation), and therapeutic exercises to reduce pain and discomfort associated with injuries, chronic conditions, or post-surgical recovery. 2. Restoring Function Physiotherapy aims to restore optimal movement patterns, strength, flexibility, and balance to help individuals regain functional independence and perform activities of daily living with ease. 3. Improving Mobility Therapists work to improve joint mobility, muscle flexibility, and range of motion, enhancing an individual’s ability to move freely and participate in physical activities without limitations. 4. Rehabilitating Injuries Physiotherapy plays a crucial role in the rehabilitation of various injuries, including sprains, strains, fractures, ligament tears, and tendonitis. Physical therapist design personalized rehabilitation programs to promote tissue healing, prevent complications, and facilitate safe return to activities. 5. Chronic Pain Management System Physiotherapy can help individuals manage chronic conditions such as arthritis, fibromyalgia, lingering pain syndromes, and neurological disorders by providing symptom relief, improving function, and enhancing quality of life. 6. Preventing Injuries Physicians educate individuals on proper body mechanics, ergonomic principles, injury prevention strategies, and exercise techniques to reduce the risk of injuries and promote long-term musculoskeletal health. Revitalize Your Health: Book a Session with Vesta Care Physiotherapists Now! How Do Physiotherapists Help Patients? Physiotherapists help patients in a variety of ways by utilizing their expertise in assessing, diagnosing, and treating a wide range of musculoskeletal, neurological, cardiopulmonary, and other conditions. Such as: a) Assessment and Diagnosis Physiotherapists conduct comprehensive assessments to evaluate a patient’s physical function, mobility, strength, flexibility, balance, and pain levels. Through thorough examination and specialized tests, they identify impairments, limitations, and contributing factors to the patient’s condition. b) Treatment Planning Based on their assessment findings and diagnosis, physicians develop individualized treatment plans tailored to the patient’s specific needs, goals, and preferences. Treatment plans may include a combination of manual therapy techniques, therapeutic exercises, modalities, education, and self-management strategies. c) Pain Management Physiotherapists utilize various techniques to alleviate pain and discomfort associated with injuries, chronic conditions, or post-surgical recovery. This may involve manual therapy techniques such as massage, joint mobilization, or therapeutic modalities such as heat, cold, electrical stimulation, or acupuncture. d) Rehabilitation Rehabilitation of injuries, surgeries, and neurological conditions by designing personalized rehabilitation programs to promote tissue healing, restore optimal movement patterns, and improve functional abilities. They guide patients through progressive exercises, mobility drills, and functional activities to facilitate recovery and regain independence. e) Education and Empowerment Patients get valuable education and self-management strategies to enhance their understanding of their condition, treatment options, and how to optimize their recovery.
At-Home Hormone Testing: Easy, Reliable, and Convenient

Hormones play a crucial role in regulating various bodily functions, from metabolism and growth to mood and reproduction. Hormone testing is a valuable tool used by healthcare providers to assess hormonal balance, diagnose conditions, and develop appropriate treatment plans. This comprehensive guide will cover everything you need to know about hormone testing, including its types, reasons for testing, how it’s done, and what the results mean. Hormones – Ready To Meet Them? Hormones are chemical messengers produced by glands in the endocrine system and released into the bloodstream. They regulate various physiological processes in the body, including metabolism, growth and development, reproduction, mood, and stress response. There are different types of hormone testing – Each type of hormone testing has its advantages and is used based on the specific hormones being evaluated and the clinical scenario. Book Appointment Why Do We Have To Test Hormones? Hormones play a vital role in regulating various bodily functions, including metabolism, growth, reproduction, and mood. Hormone testing is a crucial diagnostic tool used to assess hormone levels and identify imbalances or abnormalities that may impact health. This article provides a comprehensive overview of hormone testing, including its types, methods of testing, importance, and how it can benefit human health. Why Hormone Testing Is Crucial For Several Reasons? Technology has shaped a lot of things recently. And, it has also shaped human health. Hormone testing is essential for diagnosing endocrine disorders, managing reproductive health, monitoring hormone replacement therapy, assessing stress and adrenal function, and optimizing overall health and well-being. By providing valuable insights into hormone levels, hormone testing helps individuals and healthcare providers make informed decisions about treatment and lifestyle interventions. Here are few brief examples: 1. Diagnosis of Endocrine Disorders Hormone testing helps diagnose conditions related to hormone imbalances, such as hypothyroidism, hyperthyroidism, diabetes, adrenal insufficiency, and polycystic ovary syndrome (PCOS). By measuring hormone levels, healthcare providers can identify abnormalities and formulate appropriate treatment plans. 2. Management of Reproductive Health Hormone testing plays a vital role in assessing reproductive health, including fertility evaluations, menstrual irregularities, and menopausal symptoms. As with measuring reproductive hormones such as estrogen, progesterone, and testosterone, healthcare providers can identify factors affecting reproductive function and recommend interventions. 3. Monitoring Hormone Replacement Therapy (HRT) Individuals undergoing hormone replacement therapy, such as hormone replacement for menopause or testosterone replacement for hypogonadism, require regular hormone testing to ensure that hormone levels are within therapeutic ranges. Monitoring hormone levels helps optimize treatment efficacy and minimize potential side effects. 4. Assessment of Stress and Adrenal Function Cortisol testing, a type of hormone testing, provides insights into adrenal function and stress levels. Abnormal cortisol levels may indicate conditions such as adrenal fatigue or Cushing’s syndrome. By evaluating cortisol levels, healthcare providers can assess adrenal health and recommend appropriate interventions. 5. Optimization of Athletic Performance Hormone testing can be beneficial for athletes and fitness enthusiasts looking to optimize their performance and recovery. By measuring hormones such as testosterone, growth hormone, and cortisol, athletes can assess their hormonal profile and tailor their training regimens accordingly. Hormonal balance is important – And Here Is Why. Overall, hormone testing is essential for diagnosing endocrine disorders, managing reproductive health, monitoring hormone replacement therapy, assessing stress and adrenal function, and optimizing athletic performance. By providing valuable insights into hormone levels, hormone testing helps individuals and healthcare providers make informed decisions about their health and well-being. Don’t Forget To Book Your AT-Home Hormone Testing Appointment Today! Reasons for Hormone Testing A stitch in time saves nine is a very effective answer in this regard. However, from medical point of view here is the missing detail: 1) Hormonal Imbalance Hormone testing helps identify hormonal imbalances that may contribute to various symptoms and health issues, such as fatigue, weight gain, mood swings, and irregular menstrual cycles. 2) Diagnosis of Endocrine Disorders Hormone testing is essential for diagnosing endocrine disorders, including hypothyroidism, hyperthyroidism, diabetes, adrenal insufficiency, and polycystic ovary syndrome (PCOS). 3) Monitoring Hormone Replacement Therapy Individuals undergoing hormone replacement therapy (HRT) may require regular hormone testing to ensure optimal hormone levels and treatment efficacy. 4) Fertility Assessment Hormone testing is often performed as part of fertility evaluations to assess ovarian function, menstrual cycle regularity, and hormone levels related to ovulation. 5) Menopause Management Hormone testing can help guide treatment decisions for menopausal women, including hormone replacement therapy and symptom management. 6) Identifying Stress and Adrenal Function Cortisol, known as the stress hormone, is important for regulating the body’s response to stress. Abnormal cortisol levels can indicate conditions such as adrenal fatigue or Cushing’s syndrome, which can impact overall health and well-being. At-Home Hormone Testing Advancements in technology have made it possible for individuals to perform hormone testing at home using test kits available over-the-counter or through online providers. At-home hormone testing kits typically collect saliva or urine samples and send them to a laboratory for analysis. While convenient, at-home hormone testing may have limitations in terms of accuracy and interpretation, and it’s essential to consult with a healthcare provider for proper guidance and interpretation of results. If you have concerns about your hormone levels or symptoms suggestive of hormonal imbalances, consult with a Vesta Care healthcare provider for personalized evaluation and guidance. Call us 052 104 6920 Hormone Testing And How Is It Done? There are different ways, but here are the most common ones: I. Blood Tests: A blood sample is typically collected from a vein in the arm using a needle. The sample is then sent to a laboratory for analysis. Blood tests are the most common method of hormone testing. They measure hormone levels in the blood, providing valuable insights into hormonal imbalances or abnormalities. Different hormones, such as thyroid hormones, sex hormones (estrogen, progesterone, testosterone), adrenal hormones (cortisol, aldosterone), and pituitary hormones (growth hormone, follicle-stimulating hormone), can be assessed through blood tests. II. Saliva Tests: Saliva samples are collected using specialized collection tubes or swabs. These samples are sent to a laboratory for analysis. This testing measures the levels of hormones
The Ultimate Guide to Sustaining a Healthy Body Weight

Are you tired of fluctuating numbers on the scale and unsuccessful attempts to maintain a healthy body weight? Look no further – the ultimate guide to sustaining a healthy body weight is here to help. In this comprehensive blog, we unveil effective strategies that will empower you to achieve and maintain your weight goals. Embarking on a weight management journey can be daunting, but with the right guidance, success is within reach. Whether you have struggled with weight issues for years or simply want to adopt healthier habits, this guide is designed to equip you with the knowledge and tools you need. From nutrition tips to exercise recommendations, we leave no stone unturned. Our expert insights will demystify common misconceptions surrounding weight loss and provide evidence-based strategies that have proven results. Discover the power of mindfulness and intuitive eating, learn how to create sustainable meal plans, and find out which exercises are most effective for weight management. With this ultimate guide, you can say goodbye to fad diets and quick fixes, and instead embrace a long-term approach to a healthier, fitter you. Start your journey towards a sustainably healthy body weight today, and unlock the key to lasting success. Understanding Body Weight and Its Importance Maintaining a healthy body weight is not just about aesthetics; it is crucial for overall well-being. Understanding the significance of body weight is the first step towards effective weight management. Body weight is a measure of the total mass of an individual, including bones, muscles, organs, and fat. It serves as an indicator of the balance between energy intake and energy expenditure. When we consume more calories than we burn, the excess energy is stored as fat, leading to weight gain. On the other hand, if we consistently burn more calories than we consume, we create a calorie deficit and lose weight. Achieving a healthy body weight requires finding the right balance between these two factors. Excess body weight can have a significant impact on our health. Obesity is associated with an increased risk of various chronic conditions, including heart disease, type 2 diabetes, certain types of cancer, and joint problems. Additionally, carrying excess weight can put strain on our organs and skeletal structure, leading to decreased mobility and a reduced quality of life. Maintaining a healthy body weight not only improves physical health but also enhances mental well-being and self-confidence. It’s important to note that body weight is not solely determined by the number on the scale. Factors such as body composition, muscle mass, and overall fitness levels also play a role. Therefore, focusing solely on weight loss can be misleading. Instead, adopting a holistic approach that considers overall health and body composition is key to sustaining a healthy body weight in the long run. The Dangers of Unhealthy Body Weight Carrying excess weight can have serious implications for our health. Understanding the dangers associated with unhealthy body weight can serve as a powerful motivator to embark on a weight management journey. One of the most significant dangers of unhealthy body weight is an increased risk of developing chronic diseases. By maintaining a healthy body weight, we can significantly reduce the risk of developing these and improve overall health outcomes. Unhealthy body weight can also negatively affect mental health. Studies have shown a correlation between obesity and mental health issues such as depression and anxiety. The societal stigma surrounding excess weight can lead to low self-esteem, body image dissatisfaction, and social isolation. By achieving and sustaining a healthy body weight, we can improve our mental well-being and boost self-confidence. Furthermore, carrying excess weight can put strain on our joints and skeletal structure, leading to joint pain, osteoarthritis, and reduced mobility. This can limit our ability to engage in physical activities and adversely affect our overall quality of life. By maintaining a healthy body weight, we can alleviate the burden on our joints and improve our physical function. Factors Influencing Body Weight Body weight is influenced by a variety of factors, including genetics, metabolism, environment, and lifestyle choices. Understanding these factors can help us make informed decisions and develop effective strategies for weight management. Genetics plays a role in determining our body weight to some extent. Certain genetic variations can influence our metabolism, appetite regulation, and fat storage. However, it’s important to note that genetics are not the sole determinant of body weight. While we may have a genetic predisposition to gain or lose weight more easily, lifestyle choices and environmental factors still play a significant role. Metabolism, the process by which our bodies convert food into energy, also affects body weight. Some individuals naturally have a faster metabolism, allowing them to burn calories more efficiently. However, metabolism can be influenced by various factors, including age, gender, muscle mass, and activity level. By adopting a healthy lifestyle that includes regular physical activity and balanced nutrition, we can optimize our metabolism and support weight management. Our environment, including access to healthy food options and opportunities for physical activity, can greatly impact our body weight. Living in an obesogenic environment, characterized by the prevalence of unhealthy food choices and sedentary lifestyles, can make it more challenging to maintain a healthy body weight. However, by making conscious choices and creating a supportive environment, we can overcome these challenges and achieve our weight goals. Setting Realistic Goals for Sustainable Weight Management When it comes to weight management, setting realistic goals is crucial for long-term success. Unrealistic expectations can lead to frustration and demotivation. By setting achievable goals, we can maintain motivation and make sustainable progress. Before setting weight-related goals, it’s important to consider factors such as body composition, overall health, and lifestyle. Instead of solely focusing on the number on the scale, consider goals related to body fat percentage, strength, or overall fitness level. These goals allow for a more comprehensive approach to weight management and provide a more accurate reflection of progress. It’s also essential to set realistic timelines for achieving our goals. Rapid weight loss may
Paediatric Home Nursing for Optimal Health and Comfort

When it comes to the health and well-being of our little ones, providing quality care is of utmost importance. For parents and caregivers who want to ensure optimal health and comfort for their pediatric patients, home nursing can be a game-changer. In this guide to pediatric home nursing, we’ll explore the benefits of receiving medical care at home, the range of services available, and how to find the right healthcare professionals to provide the best care for your child. Pediatric home nursing allows children with complex medical needs to receive the care they require in the comfort and familiar surroundings of their own home. With a team of skilled nurses and caregivers, children can receive personalized and comprehensive care, tailored to their specific needs. From administering medications and managing chronic conditions to providing emotional support, pediatric home nurses play a crucial role in improving a child’s overall well-being. This guide will provide valuable information and resources for parents and caregivers considering pediatric home nursing as an option for their child’s care. By understanding the benefits, services, and how to find the right professionals, you can ensure your child receives the quality care they deserve in the place they feel most comfortable – home. Benefits of Paediatric Home Nursing Pediatric home nursing offers numerous benefits for both children and their families. Firstly, being cared for at home allows children to remain in a familiar environment, reducing stress and anxiety. This familiarity can have a positive impact on their emotional well-being and overall comfort. Additionally, home nursing eliminates the need for frequent hospital visits, minimizing exposure to potential infections and reducing the risk of hospital-acquired illnesses. Furthermore, pediatric home nursing provides the opportunity for personalized care. Each child is unique, and their medical needs require individual attention. Home nurses work closely with the child’s healthcare team to develop personalized care plans that address their specific needs, ensuring that they receive the best possible care. In addition to personalized care, pediatric home nursing also enables family involvement in the child’s care. Parents and caregivers play an active role in the child’s treatment, working closely with the home nurse to provide support and assistance. This collaboration fosters a sense of empowerment and strengthens the bond between the child and their caregivers. Common Conditions Requiring Paediatric Home Nursing Pediatric home nursing caters to a wide range of medical conditions, providing specialized care for children with complex healthcare needs. Some common conditions that may require pediatric home nursing include: Chronic respiratory conditions: Children with chronic respiratory conditions such as asthma, cystic fibrosis, or bronchopulmonary dysplasia often require ongoing monitoring and support. Home nurses can help manage respiratory therapies, administer medications, and educate parents on symptom management. Neurological disorders: Children with neurological disorders, such as cerebral palsy or epilepsy, may require specialized care to manage their condition. Pediatric home nurses can assist with seizure management, administer medications, and provide support to both the child and their family. Gastrointestinal conditions: Children with gastrointestinal conditions, like Crohn’s disease or short bowel syndrome, may require enteral or parenteral nutrition at home. Home nurses can assist in the administration and monitoring of these specialized nutrition therapies. Cardiac conditions: Children with congenital heart defects or other cardiac conditions may require ongoing monitoring and support. Pediatric home nurses can help with cardiac assessments, assist in the management of medications, and provide education to parents on caring for their child’s heart condition. These are just a few examples of the conditions that pediatric home nursing can address. Each child’s needs are unique, and the care provided is tailored to their specific condition and requirements. The Role of a Paediatric Home Nurse Pediatric home nurses play a vital role in the care of children with complex medical needs. They bring a wealth of knowledge and expertise to ensure the well-being of their young patients. Here are some key responsibilities of a pediatric home nurse: Medical assessments: Home nurses perform regular medical assessments to monitor the child’s health status, identify any changes or concerns, and make appropriate interventions. Medication administration: Administering medications is a crucial aspect of pediatric home nursing. Home nurses ensure that medications are administered correctly, monitor for any adverse reactions, and educate parents on medication management. Wound care: For children with wounds or surgical incisions, home nurses provide wound care, including dressing changes, infection prevention, and monitoring for any signs of complications. Coordination of care: Pediatric home nurses collaborate with the child’s healthcare team, including doctors, therapists, and other specialists, to ensure seamless coordination of care. They communicate updates, share information, and advocate for the child’s needs. Emotional support: Pediatric home nurses provide emotional support not only to the child but also to the parents and caregivers. They offer reassurance, listen to concerns, and provide guidance to help families navigate the challenges of caring for a child with complex medical needs. Creating a Safe and Comfortable Environment for Paediatric Home Nursing Creating a safe and comfortable environment is essential for pediatric home nursing. Here are some tips to ensure the best possible environment for your child’s care: Childproofing: Make sure your home is childproofed, removing any potential hazards and ensuring a safe space for your child. This includes securing electrical outlets, installing safety gates, and keeping dangerous substances out of reach. Comfortable sleeping arrangements: Create a comfortable sleeping area for your child, ensuring they have a supportive mattress, appropriate bedding, and a soothing sleep environment. Accessible medical supplies: Keep all necessary medical supplies readily accessible and organized. This includes medications, dressings, feeding tubes, and any other equipment specific to your child’s needs. Maintain cleanliness: Regularly clean and disinfect the areas where your child receives care. This helps prevent the spread of germs and reduces the risk of infections. Emergency preparedness: Have an emergency plan in place, including contact numbers for healthcare providers, ambulance services, and nearby hospitals. Ensure that all caregivers are aware of the plan and know how to respond in case of an emergency. By creating a safe and comfortable
The Benefits of Physiotherapy at Home: Stay Active and Pain-Free

Are you tired of dealing with chronic pain or recovering from an injury? Physiotherapy could be the solution you’ve been searching for. And the best part? You can now access the benefits of physiotherapy right from the comfort of your own home. With the rise of home healthcare services, you can receive personalized treatment and guidance from a qualified physiotherapist without leaving your living room. Physiotherapy at home offers numerous advantages. It allows you to maintain an active lifestyle and stay pain-free while avoiding the hassle and expense of commuting to a clinic. Whether you’re looking to manage chronic pain, improve your flexibility, or recover from a sports injury, physiotherapy can help. Through a combination of exercises, stretches, and other therapeutic techniques, a qualified physiotherapist can create a tailored treatment plan to address your specific needs. Unlock the benefits of physiotherapy at home and take control of your health and well-being. Say goodbye to pain and discomfort and hello to a more active, pain-free life. Book an appointment with a us today and start your journey towards a stronger, healthier body. Benefits of physiotherapy at home Physiotherapy at home offers numerous advantages. It allows you to maintain an active lifestyle and stay pain-free while avoiding the hassle and expense of commuting to a clinic. One of the key benefits of physiotherapy at home is convenience. You can schedule your sessions at a time that suits you best, without having to worry about traffic or long waiting times. This flexibility makes it easier to incorporate physiotherapy into your daily routine. Another advantage is the personalized attention you receive from a qualified physiotherapist. During home sessions, the physiotherapist can focus solely on your needs and tailor the treatment plan accordingly. This personalized approach ensures that you get the most effective treatment for your specific condition, whether it’s managing chronic pain, improving flexibility, or recovering from a sports injury. Physiotherapy at home also allows for a comfortable and familiar environment. Being in your own home can help you feel more relaxed and at ease during the sessions, which can contribute to better outcomes. Furthermore, being surrounded by your own belongings and having easy access to any necessary equipment or aids can enhance the effectiveness of the treatment. Common conditions treated with physiotherapy at home Physiotherapy at home can be beneficial for a wide range of conditions. One common condition that can be effectively managed through home physiotherapy is lower back pain. Whether it’s caused by poor posture, muscle strain, or a herniated disc, a qualified physiotherapist can design a treatment plan that includes exercises and stretches to strengthen the muscles, improve flexibility, and alleviate pain. Another condition that can benefit from home physiotherapy is osteoarthritis. This degenerative joint disease can cause pain, stiffness, and reduced range of motion. With the guidance of our physiotherapist, you can learn exercises and techniques to improve joint mobility, strengthen supporting muscles, and manage pain. The goal is to enhance your quality of life and enable you to engage in daily activities with ease. Sports injuries are also commonly treated through physiotherapy at home. Whether you’re a professional athlete or a weekend warrior, injuries can happen. By working with a physiotherapist, you can receive targeted treatment that focuses on restoring function, reducing pain, and preventing future injuries. The physiotherapist will create a customized rehabilitation plan that may include exercises, manual therapy, and other modalities to help you recover and get back to your sport as quickly and safely as possible. How to find a qualified physiotherapist near you? Finding a qualified physiotherapist for home visits is crucial to ensure you receive the best possible care. You can also search online directories and find companies like ours or use platforms that connect you with qualified physiotherapists who offer home visits. Make sure to check their credentials, experience, and any reviews or testimonials from previous patients. It’s important to find a physiotherapist who specializes in your specific condition or injury to ensure you receive the most effective treatment. Our physiotherapists are all licensed by DHA and have ample experience in a range of services. What to expect during a home physiotherapy session When you schedule a home physiotherapy session, our physiotherapist will typically start by conducting an initial assessment. This assessment may include a detailed discussion about your medical history, current symptoms, and goals for treatment. The physiotherapist may also perform physical tests to evaluate your range of motion, strength, and flexibility. Based on the assessment, the physiotherapist will create a personalized treatment plan tailored to your specific needs. This plan may include a combination of exercises, stretches, manual therapy techniques, and other modalities. The physiotherapist will guide you through each exercise and provide feedback and corrections to ensure proper form and technique. During the sessions, the physiotherapist will monitor your progress, adjust the treatment plan as needed, and provide education and advice on self-management techniques. They may also recommend modifications to your daily activities or suggest assistive devices to help you manage your condition more effectively. Exercises and techniques used in home physiotherapy Home physiotherapy can involve a variety of exercises and techniques depending on your condition and goals. Strengthening exercises are commonly used to improve muscle function and stability. These exercises can target specific muscle groups or focus on overall body strength. The physiotherapist will guide you through each exercise and gradually increase the difficulty as you progress. Stretching exercises are also an important component of home physiotherapy. They help improve flexibility, increase range of motion, and reduce muscle tension. The physiotherapist will teach you stretching techniques that target the affected areas and provide instructions on how to perform them correctly. In addition to exercises, manual therapy techniques may be used during home physiotherapy sessions. These techniques involve the hands-on manipulation of muscles, joints, and soft tissues to reduce pain, improve mobility, and promote healing. The physiotherapist will apply specific techniques based on your condition and individual needs. Other modalities that may be used in home physiotherapy
HIV Risk: What You Need to Know in Dubai

Even while there is little chance of transmission through routine activities and ambient surfaces, there are a few things to be aware of. In the event that non-sterile equipment is used for procedures like body piercing and tattooing, there is a potential danger. In Dubai’s dynamic and diverse environment, education on safe practices and cleanliness measures are critical in reducing HIV risks. HIV And Pathogenesis! HIV or human deficiency virus is a type of virus that attacks immune cells that help fight body infection. They help to fight against infection, also prevent a person from becoming sick and regulate your normal body response during any kind of pathogen invasion or viral invasion. The human immunodeficiency virus is a specific virus that causes a deadly disease known as acquired immunodeficiency syndrome. Which is a bucket of several infections that affect the human body drastically. HIV attacks and destroys the infection-fighting CD-4 immune cells making the body vulnerable and unable to fight off infection which results in the reduction of your normal body’s immune response resulting in a high infection rate and certain cancers. HIV gradually destroys the immune system causing a decline in the normal immunity and onset of AIDS. Mode of Transmission HIV can be transmitted from one person to another when certain bodily fluids are shared between people. Bodily fluids that can transmit HIV include blood, semen, pre-seminal fluid, vaginal fluids, rectal fluids, and breast milk. HIV can be transmitted during vaginal or anal sex, through sharing needles for injecting drugs or tattooing, by getting stuck with a needle that has the blood of someone with HIV on it, through pregnancy, and breastfeeding. A HIV-positive individual who during pregnancy, childbirth, or lactation spreads the virus to their offspring. Nonetheless, the risk of HIV transmission during pregnancy. Signs and symptoms Once you have HIV, you may have a number of symptoms, such as fever, chills, and night sweats along with anxiety and sadness. Mouth ulcers can also be caused by heart problems, neuropathy, hypertension, diarrhea, and weakened immune systems. The disease’s capacity to spread infections like Kaposi sarcoma is caused by the virus’s ability to replicate. Risk Understanding Understanding the HIV risk in this way required a comprehensive approach to preventive measures, local Healthcare resources and a commitment to safe practice. In Dubai, there are a lot of different healthcare service providers that are readily available for HIV testing counseling and treatment. Individuals should take advantage of these resources to get regular screening, especially if anyone is engaged in behavior. 1. Sexual Intercourse Having sex without a condom greatly raises the risk of HIV infection. By acting as a barrier, condoms stop the spread of bodily fluids that could be infected with the virus. One important preventive measure is to use condoms correctly and consistently. 2. Sexually Transmitted Infection Containing Intercourse People who already have a STI, such as bacterial vaginosis, herpes, chlamydia, gonorrhea, or syphilis, are more vulnerable to HIV. HIV can enter the body through vaginal sores, inflammation, and tears in the skin or mucous membranes caused by these illnesses. 3. Sharing Contaminated Needles and Drug Equipment Sharing syringes, needles, or other drug-related items when injecting drugs greatly increases the risk of HIV transmission. The virus can be present in blood and can easily be transmitted through the sharing of contaminated equipment during drug use. 4. Accidental Needlestick Injuries Needlestick injuries, especially those sustained by medical personnel, carry the potential to spread HIV. The virus can enter the circulation accidentally through contact with contaminated needles or sharp items, which highlights the significance of managing and discarding medical equipment properly. 5. Oral Intercourse Although there is less chance of HIV transmission through oral sex than through anal or vaginal intercourse, it is nevertheless present. If there are cuts or open sores in the mouth or genitalia, the danger goes up. The risk can be decreased by using barriers during oral intercourse, such as condoms or dental dams. 6. Blood transfusions and organ transplants The risk of HIV transmission during organ transplants and blood transfusions has been considerably decreased by rigorous screening, but it’s crucial to remember that the risk still exists. Sustained improvements in safety procedures are necessary to reduce this possible danger even more. 7. Equipment for Intravenous Drug Use If shared blood is contaminated with cookers or cotton, it might spread HIV. Needles are not the only equipment that can be used for intravenous drug use. However, sharing needles carries the biggest risk. 8. Unsafe Medical Practices People can get HIV from receiving unsafe injections, blood transfusions, tissue transplants, and medical operations involving piercing or cutting without sterility. In order to stop transmission, proper sterilization and infection control procedures are essential in medical environments. 9. Saliva and HIV Saliva poses a very minimal risk of HIV transmission but includes enzymes that suppress the virus, and the viral concentration in saliva is often insufficient for transmission. However, there have been extremely rare occurrences documented, usually with considerable bleeding and sores. 10. Occupational Exposure Healthcare personnel face a relatively low risk of contracting HIV through incidental contact with body fluids, thanks to rigorous infection control measures. The use of protective equipment further minimizes this risk, providing an additional layer of defense. In the event of inadvertent exposure, healthcare professionals can benefit from post-exposure prophylaxis (PEP), a preventive treatment that plays a crucial role in safeguarding their well-being and ensuring a prompt and effective response to potential HIV exposure. 11. Tattooing and Body Piercing Using unsterilized needles or equipment during body piercings and tattoos carries a potential risk of HIV transmission if they come into contact with contaminated blood, while this risk is thought to be very low. Sterilization procedures and diligent hygiene compliance greatly reduce this risk. Through a focus on hygiene and the use of appropriate sterilizing techniques, healthcare professionals improve safety and reduce the risk of HIV infection. 12. Contact with Environmental Surfaces The risk of HIV transmission from environmental surfaces, such as counters and toilets,
Understanding Chlamydia: The Silent Threat in Sexual Health
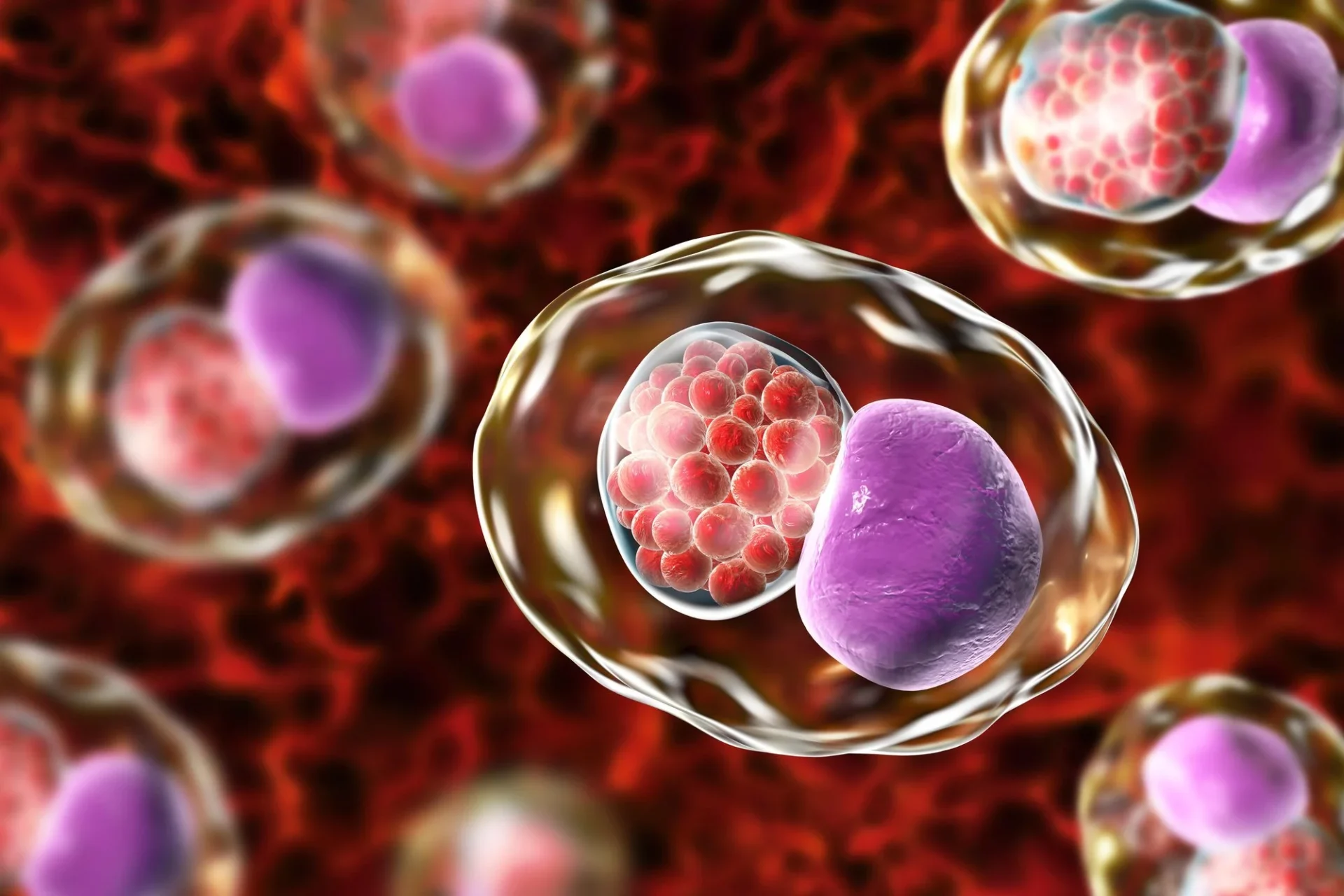
In today’s fast-paced world, it’s easy to overlook the silent threats that lurk in our sexual health. One such threat is the prevalent and often asymptomatic infection known as Chlamydia. With its sneaky nature, Chlamydia silently spreads, affecting millions worldwide. But what exactly is Chlamydia and why is it a concern? This article aims to shed light on this commonly misunderstood sexually transmitted infection (STI). Chlamydia is caused by the bacterium Chlamydia trachomatis and can be transmitted through sexual activity, including vaginal, anal, and oral sex. What makes it especially concerning is the fact that it often presents no symptoms, leading many to remain unaware of their infection. Left untreated, Chlamydia can have severe consequences, including fertility issues and an increased risk of other STIs. By understanding Chlamydia, its transmission, symptoms (or lack thereof), and the importance of regular testing and treatment, we can empower ourselves with the knowledge necessary to protect our sexual health. Join us as we delve into the world of Chlamydia and equip ourselves with the information needed to combat this silent threat. What is Chlamydia? Chlamydia is caused by the bacterium Chlamydia trachomatis and can be transmitted through sexual activity, including vaginal, anal, and oral sex. It is one of the most common STIs globally, with millions of new cases reported each year. What makes Chlamydia especially concerning is the fact that it often presents no symptoms, leading many to remain unaware of their infection. This silent nature of Chlamydia can contribute to its widespread transmission and long-term health consequences if left untreated. Chlamydia is primarily transmitted through unprotected sexual contact with an infected individual. The bacteria can infect the urethra, cervix, rectum, or throat. It can also be passed from an infected mother to her baby during childbirth. While Chlamydia can affect anyone, young people, particularly those between the ages of 15 and 24, are at a higher risk of infection. Prevalence and impact of Chlamydia Chlamydia is a global health concern, with millions of new cases reported each year. According to the World Health Organization (WHO), an estimated 127 million new cases of Chlamydia occur annually. However, this number likely underestimates the true prevalence, as many cases go undiagnosed and unreported due to the lack of symptoms. The impact of Chlamydia goes beyond the immediate discomfort and inconvenience it may cause. Untreated Chlamydia can have severe consequences, especially for women. In women, Chlamydia can lead to pelvic inflammatory disease (PID), which can cause chronic pelvic pain, infertility, and an increased risk of ectopic pregnancy. In men, untreated Chlamydia can result in epididymitis, which can lead to testicular pain and, in rare cases, infertility. Signs and symptoms of Chlamydia One of the concerning aspects of Chlamydia is that it often presents no symptoms or mild symptoms that can easily be mistaken for other conditions. This means that many individuals may unknowingly carry and transmit the infection. When symptoms do occur, they typically manifest within one to three weeks after exposure. Common symptoms in women include abnormal vaginal discharge, pain during urination, and abdominal or pelvic pain. Men may experience discharge from the penis, burning or itching sensation during urination, and testicular pain. However, it’s important to note that these symptoms can vary or be absent altogether, making regular testing crucial for early detection and treatment. How is Chlamydia diagnosed? Diagnosing Chlamydia involves various methods, including laboratory testing. The most common diagnostic method is a urine test, which can detect the presence of Chlamydia DNA. Additionally, swabs may be taken from the cervix, urethra, rectum, or throat to collect samples for testing. These samples are then analyzed in a laboratory to determine the presence of Chlamydia. It’s important to remember that routine testing for Chlamydia is not typically included in regular check-ups or screenings, unless specifically requested. Individuals who are sexually active, particularly those with multiple partners or who engage in unprotected sex, should proactively seek testing to ensure early detection and treatment if necessary. Potential complications of untreated Chlamydia While Chlamydia may seem like a relatively harmless infection due to its lack of symptoms, untreated Chlamydia can lead to serious health complications. As mentioned earlier, women are particularly at risk for developing pelvic inflammatory disease (PID), which can cause long-term damage to the reproductive organs and increase the chances of infertility. In some cases, Chlamydia can also increase the risk of miscarriage or preterm birth. For men, untreated Chlamydia can result in epididymitis, a painful condition that affects the epididymis, the tube that carries sperm from the testicles. If left untreated, epididymitis can lead to testicular abscesses or even permanent damage to the reproductive system. Preventing Chlamydia transmission Preventing Chlamydia transmission requires a combination of safe sexual practices, open communication, and regular testing. The use of barrier methods, such as condoms or dental dams, can significantly reduce the risk of Chlamydia transmission during sexual activity. It’s important to note that while condoms provide a level of protection, they do not eliminate the risk entirely, as Chlamydia can be present in areas not covered by the condom. Open and honest communication with sexual partners is also crucial in preventing the spread of Chlamydia. Discussing sexual health, previous STI testing, and using protection can help reduce the risk of infection. Regular testing is key to early detection and treatment of Chlamydia. Testing should be done regularly, especially for individuals with multiple sexual partners or those who engage in unprotected sex. It’s also important to note that Chlamydia can be present in areas not typically associated with sexual activity, such as the throat or rectum. Therefore, individuals engaging in oral or anal sex should also consider getting tested regularly. Treatment options for Chlamydia Fortunately, Chlamydia is a treatable infection. The most common treatment for Chlamydia is a course of antibiotics, typically taken orally. It’s crucial to complete the full course of antibiotics as prescribed, even if symptoms improve or disappear before completing the treatment. This ensures the complete eradication of the infection and reduces the risk
Unraveling the Low-Carb vs. Low-Fat Debate for a Solution

Are you confused about whether to go low-carb or low-fat for weight loss? The debate between low-carb and low-fat diets has been ongoing for years, leaving many people unsure which approach is right for them. In this article, we’ll decode the food choices, unravel the complexities of the low-carb versus low-fat debate, and help you make an educated decision. Both low-carb and low-fat diets have their benefits and drawbacks. Low-carb diets focus on reducing carbohydrate intake, while low-fat diets prioritize cutting back on fat consumption. The key to finding the right solution lies in understanding the science behind these dietary approaches and how they impact our bodies. With the help of experts in the field, we’ll explore the pros and cons of both low-carb and low-fat diets, as well as their effects on weight loss, heart health, and overall well-being. By the end of this article, you’ll have the knowledge and confidence to make informed food choices that align with your health goals. Don’t let the low-carb versus low-fat debate leave you feeling overwhelmed. Let’s unravel the complexities together and find the right solution for you. Understanding the low-carb vs. low-fat debate When it comes to the low-carb versus low-fat debate, it’s essential to understand the fundamental differences between these two dietary approaches. Low-carb diets, such as the popular ketogenic diet, restrict carbohydrate intake to induce a state of ketosis, where the body burns fat for fuel instead of carbohydrates. On the other hand, low-fat diets emphasize reducing the intake of dietary fats, including saturated and trans fats, in an effort to lower calorie consumption and promote weight loss. The dual nature of obesity: Medical and social implications Obesity is not just a medical issue; it is also a social problem that affects individuals on multiple levels. From a medical perspective, obesity is associated with a wide range of health complications, including cardiovascular disease, diabetes, and certain types of cancer. Excess weight puts a strain on the body’s systems, leading to increased risks and decreased quality of life. However, the effects of obesity extend beyond physical health. Socially, individuals who are obese often face discrimination, stigma, and prejudice. They may be subjected to body shaming, bullying, and exclusion. These negative experiences can have a profound impact on mental health, leading to low self-esteem, depression, and anxiety. The social implications of obesity are wide-ranging and can affect various aspects of life, including relationships, education, and employment opportunities. To truly address the issue of obesity, it is essential to recognize and address both the medical and social implications. By adopting a holistic approach that takes into account the interconnectedness of these factors, we can create a supportive environment that promotes overall well-being and empowers individuals to overcome obesity. The science behind low-carb diets Low-carb diets have gained significant attention for their potential weight loss benefits. By limiting carbohydrate intake, the body is forced to use fat stores for energy, leading to weight loss. Additionally, low-carb diets may help stabilize blood sugar levels, improve insulin sensitivity, and reduce cravings for sugary foods. However, it’s important to note that not all carbohydrates are created equal, and a well-rounded low-carb diet should focus on consuming nutrient-dense, high-fiber sources of carbohydrates. Despite their potential benefits, low-carb diets also have some drawbacks. They can be challenging to sustain in the long term, as they often restrict or eliminate certain food groups, such as grains, legumes, and fruits. This can lead to nutrient deficiencies if not carefully planned. Additionally, for individuals with certain medical conditions, such as kidney disease, a low-carb diet may not be suitable. The science behind low-fat diets On the other side of the debate, low-fat diets have been a popular approach to weight loss for many years. By reducing fat intake, individuals can lower overall calorie consumption and potentially achieve weight loss. Low-fat diets often emphasize consuming lean proteins, whole grains, fruits, vegetables, and low-fat dairy products. These foods provide essential nutrients while keeping saturated and trans fat intake to a minimum. Low-fat diets have been associated with improvements in heart health, as they can help reduce levels of LDL cholesterol and triglycerides. They may also lower the risk of certain chronic diseases, such as cardiovascular disease and type 2 diabetes. However, it’s important to note that not all fats are unhealthy, and a well-rounded low-fat diet should still include sources of healthy fats, such as nuts, seeds, avocados, and fatty fish. Pros and cons of low-carb diets Like any dietary approach, low-carb diets have their share of pros and cons. On the positive side, low-carb diets have shown promising results for weight loss, especially in the short term. They can also improve markers of metabolic health, such as blood sugar and insulin levels. Low-carb diets may help reduce hunger and cravings, making it easier to stick to a calorie deficit. However, they can be challenging to maintain in the long term, especially for individuals who enjoy a variety of foods or have specific dietary restrictions. It’s important to consider individual preferences and lifestyle factors when deciding if a low-carb diet is right for you. Pros and cons of low-fat diets Similarly, low-fat diets have their own set of advantages and disadvantages. On the positive side, low-fat diets can be more flexible and easier to sustain in the long term, as they allow for a wider variety of foods. They can also promote heart health by reducing saturated and trans fat intake. However, low-fat diets may not be as effective for weight loss as low-carb diets, and some individuals may find it challenging to achieve satiety without sufficient fat intake. It’s crucial to consider personal preferences and goals when deciding if a low-fat diet is the right choice. Finding the right balance: a flexible approach to food choices Rather than getting caught up in the low-carb versus low-fat debate, it’s essential to find a balance that works for you. The ideal approach may involve incorporating elements of both low-carb and low-fat principles while
Overcoming Obesity: Tackling Medical and Social Challenge

In today’s society, obesity has become a dual medical and social challenge that affects millions of people worldwide. The struggle to combat this epidemic requires a holistic approach that goes beyond just diet and exercise. This article explores the various aspects of overcoming obesity, addressing both the physical and mental factors that contribute to weight gain. With the rising numbers of individuals grappling with weight issues, it has become imperative to adopt a holistic approach to overcome obesity. In this article, we shed light on the intertwined medical and social aspects of obesity. As we delve into this topic, we aim to empower you with knowledge and practical strategies to conquer this pervasive challenge. From understanding the underlying health conditions associated with obesity to exploring the psychological factors that contribute to weight gain, we leave no stone unturned. Join us on this informative journey as we navigate through the obstacles and provide insights on how to transform your lifestyle. By adopting a holistic approach, we can pave the way towards a healthier, happier, and more fulfilling life. Get ready to take charge of your well-being and embark on a transformative journey towards overcoming obesity. Understanding obesity: Causes and consequences Obesity is a multifaceted condition that results from a combination of genetic, environmental, and behavioral factors. While genetics play a role in predisposing individuals to obesity, it is the environment and lifestyle choices that predominantly contribute to weight gain. Sedentary lifestyles, poor dietary habits, and an abundance of processed foods have fueled the obesity epidemic. Additionally, certain medical conditions, such as hypothyroidism and polycystic ovary syndrome (PCOS), can also lead to weight gain. The consequences of obesity are far-reaching and impact not only physical health but also mental and emotional well-being. Obesity increases the risk of developing chronic conditions such as heart disease, type 2 diabetes, and certain cancers. It can also lead to reduced mobility, joint pain, and sleep apnea. Moreover, the social and psychological consequences of obesity, such as discrimination, low self-esteem, and depression, further exacerbate the challenges faced by individuals struggling with their weight. In order to combat obesity effectively, it is crucial to understand its causes and consequences. By gaining insight into the factors that contribute to weight gain and the impact it has on overall health and well-being, we can develop a holistic approach to tackle this dual medical and social challenge. The dual nature of obesity: Medical and social implications Obesity is not just a medical issue; it is also a social problem that affects individuals on multiple levels. From a medical perspective, obesity is associated with a wide range of health complications, including cardiovascular disease, diabetes, and certain types of cancer. Excess weight puts a strain on the body’s systems, leading to increased risks and decreased quality of life. However, the effects of obesity extend beyond physical health. Socially, individuals who are obese often face discrimination, stigma, and prejudice. They may be subjected to body shaming, bullying, and exclusion. These negative experiences can have a profound impact on mental health, leading to low self-esteem, depression, and anxiety. The social implications of obesity are wide-ranging and can affect various aspects of life, including relationships, education, and employment opportunities. To truly address the issue of obesity, it is essential to recognize and address both the medical and social implications. By adopting a holistic approach that takes into account the interconnectedness of these factors, we can create a supportive environment that promotes overall well-being and empowers individuals to overcome obesity. The importance of a holistic approach to tackling obesity When it comes to overcoming obesity, a one-size-fits-all approach simply does not work. Each individual’s journey towards weight loss and improved health is unique, requiring a comprehensive and personalized approach. This is where a holistic approach comes into play. By addressing the various aspects of obesity, including physical, mental, and social factors, we can create a roadmap for lasting change. A holistic approach to tackling obesity involves looking at the individual as a whole, rather than focusing solely on weight loss. It takes into account the underlying causes of weight gain, such as unhealthy eating patterns, sedentary lifestyles, and emotional eating. Additionally, it considers the impact of mental and emotional well-being on weight management. By addressing these factors, we can develop a sustainable plan that not only helps individuals shed excess pounds but also promotes long-term health and well-being. A holistic approach also emphasizes the importance of self-care and self-compassion. It encourages individuals to cultivate a positive relationship with their bodies, focusing on nourishing and nurturing themselves rather than punishing or depriving themselves. This shift in mindset is crucial for long-term success and helps individuals develop a healthy and sustainable relationship with food and exercise. In the following sections, we will explore the key components of a holistic approach to tackling obesity. From nutrition and diet to physical activity and exercise, as well as mental health and community support, we will provide you with practical strategies and insights to guide you on your journey towards overcoming obesity. Nutrition and diet: obesity Key factors in managing Proper nutrition and a healthy diet are foundational elements in managing obesity. A balanced diet that is rich in nutrient-dense foods is essential for weight loss, as it provides the body with the necessary nutrients while keeping calorie intake in check. One of the key principles of a healthy diet is portion control. It is important to be mindful of portion sizes and to listen to your body’s hunger and fullness cues. This can be achieved by practicing mindful eating, which involves paying attention to the taste, texture, and satisfaction derived from food. By slowing down and savoring each bite, you can better gauge your body’s signals and prevent overeating. In addition to portion control, the quality of food is also crucial. Opt for whole, unprocessed foods that are rich in nutrients and low in added sugars and unhealthy fats. Include a variety of fruits, vegetables, whole grains, lean proteins, and healthy
